What are the signs and symptoms of SPD?
SPD has a lot of signs and symptoms but all of these symptoms may or may not appear altogether. SPD symptoms are grouped into the following:
People suffering from over-responsivity might:
Dislike textures such as those found in fabrics, foods, grooming products or other materials found in daily living, to which most people would not react. This dislike interferes with normal function.
Avoid crowds and noisy places
Motion sickness (not related to other medical explanations)
Refuse normal skin contact interactions (kissing, cuddling or hugging) due to negative experience of touch sensation (not to be confused with shyness or social difficulties)
Feel seriously discomforted, sick or threatened by normal sounds, lights, movements, smells, tastes, or even inner sensations such as heartbeat.
Be picky eaters
Have sleep disorders (waking up to minor sounds, problems getting sleep because of sensory overload)
Find it difficult to self calm, feel constantly under stress
People suffering from under-responsivity:
Show extreme difficulties waking up
Appear unreactive and slow
Be unaware of pain and/or other people
Might appear deaf even when auditory function has been tested
Child might be difficult being toilet trained, unaware of being wet or soiled
People suffering from sensory craving might:
Fidget excessively
Seek or make loud, disturbing noises
Climb, jump and crash constantly
Seek “extreme” sensations
Suck on or bite clothing, fingers, pencils, etc.
Appear impulsive
People suffering from sensory motor based problems might:
Appear slow and uncoordinated
Feel clumsy, slow, poor motor skills or handwriting
Have poor posture
Children might be delayed in crawling, standing, walking or running
Become verbose to avoid motor tasks
People suffering from sensory discrimination problems might:
Drop things constantly Have poor handwriting
Difficulty dressing and eating Use inappropriate force to handle objects
Other signs and symptoms:
Poorly integrated balance and rightening reflexes
Low muscle tone patterns
Poor core tone
Low postural control (may appear hunchback)
Poor nystagmus (or involuntary eye movement)
Presence of non integrated reflexes
Jerky eye tracking
Poor tactile astereognosis (inability to identify an object by active touch of the hands without other sensory input) Inadequate motor, ideational or constructional praxis
Difficulties with planning movement using feedback information
Difficulties with planning movement using feedforward information
Poor motor coordination
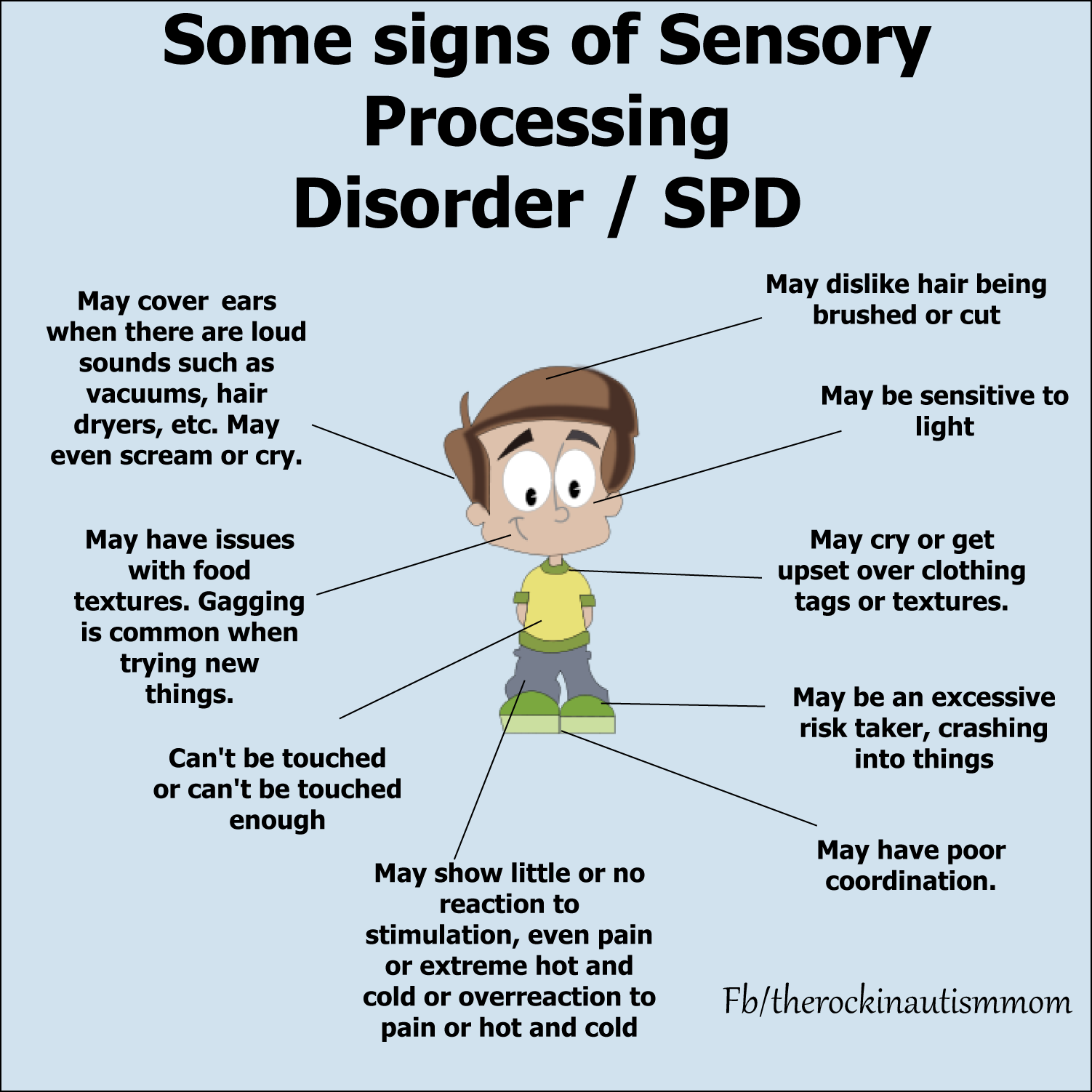
Image courtesy of rockinmomsworld.wordpress.com.
Diagram of SPD symptoms
How is SPD treated?
Therapies are used to treat SPD:
Sensory integration therapy – in this therapy, the therapist works closely with the child to provide a level of sensory stimulation that the child can cope with, and encourage movement within the room. Sensory integration therapy is driven by four main principles:
Just right challenge (the child must be able to successfully meet the challenges that are presented through playful activities)
Adaptive response (the child adapts his behavior with new and useful strategies in response to the challenges presented)
Active engagement (the child will want to participate because the activities are fun)
Child directed (the child’s preferences are used to initiate therapeutic experiences within the session)
Sensory processing therapy – the same as sensory integration therapy but adds the following: Intensity (person attends therapy daily for a prolonged period of time) Developmental approach (therapist adapts to the developmental age of the person, against actual age) Test-retest systematic evaluation (all clients are evaluated before and after) Process driven vs. activity driven (therapist focuses on the “Just right” emotional connection and the process the reinforces the relationship) Parent education (parent education sessions are scheduled into the therapy process) “joie de vivre” (happiness of life is therapy’s main goal, attained through social participation, self-regulation, and self-esteem) Combination of best practice interventions (is often accompanied by integrated listening system therapy, floor time, and electronic media such as Xbox Kinect, Nintendo Wii, Makoto II machine training and others) Developmental, Individual
Difference, Relationship-based (DIR) model – developed by Stanley Greenspan, MD, and Serena Wieder, PhD, where parents are first asked to follow the child’s lead, even if the playtime behavior isn’t typical. For example, if a child is rubbing the same spot on the floor over and over, the parent does the same. These actions allow the parent to “enter” into the child’s world.[17] This is followed by a second phase, where parents use the play sessions to create challenges for the child. The challenges help pull the child into what Greenspan calls a “shared” world with the parent. And the challenges create opportunities for the child to master important skills in areas such as[17]: Relating Communicating Thinking
A major part of this therapy is the “floortime” method. The method involves multiple sessions of play with the child and parent. The play sessions last about 20 minutes.
My Favorite:
The Listening Program

The function of the ear is to feel and hear sounds and movement. It is referred to as the vestibular-cochlear system. The cochlea is the part of the ear that is our hearing sense organ, responding to minute vibrations and differences in sound waves. The vestibular portion of the ear detects movement of the head in space. It is considered the organizer of our body senses. It is our internal ear, allowing us to understand time and space from our body’s perspective. It has a strong impact on muscle tone, posture, balance, coordination, integration of the two body sides, visual spatial skills, emotional responses and motor-planning.
The vestibular-cochlear system is the first to develop in the utero and provides the foundation for both time and space organization of all other sensory systems. Therapeutic Listening® treatment stimulates and exercises the vestibular-cochlear system. It is designed to enhance the accuracy of the sensory information sent from the vestibular-cochlear system of the ear to its multiple connections throughout the nervous system.
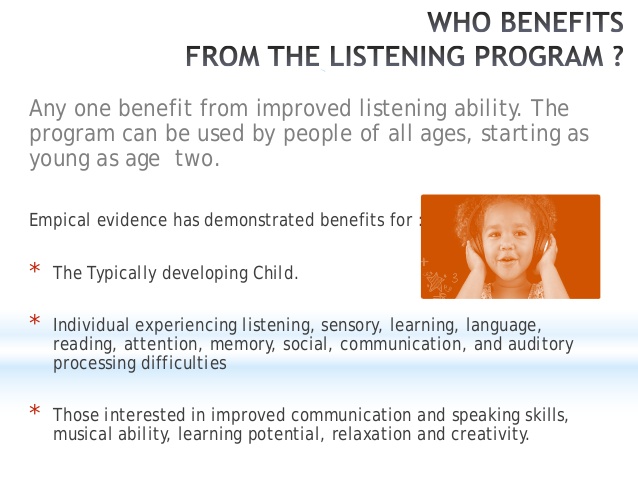
TLP is reknown for benifiting individuals with the following difficulties:
Regulating sleep patterns
Restricted diet and eating patterns/habits
Reduced attention and difficulties sustaining concentration for tasks e.g. school work
Communication difficulties, delayed speech development
Regulating emotional and behavioural responses e.g. tantrums, anxiety, flattened emotional responses/expressions
Irregularities in toilet training
Reduced social skills, engagement and reduced self-esteem & confidence
Delayed or awkward motor skills; coordination, planning and balance
Handwriting difficulties
Visual perceptual difficulties
Disorganisation, impulsive behaviours or anxiety
Autism, Aspergers and ADD/ADHD
Sensory Processing Disorders
Downs Syndrome
Learning Difficulties
This approach builds on all of the scientific knowledge about sensory-motor integration as CNS organizer for meaningful function. The Listening Program® (TLP) includes the addition of music through the use of electronically altered music and natural sounds to impact the central nervous system. This addition of music ties brainstem integration together with limbic system integration leading to more organized and functional behaviour outcomes. The addition of the auditory system to this treatment equation provides the considerable and unique power of uniting brainstem, limbic system, and cerebral cortex in the support of the development and emergence of higher cortical and cognitive function.
Information adapted from Steven J. Cool, PhD, FAAO in Vitallinks Newsletter 2004.
What are the benefits of The Listening Program®?
When TLP is coupled with a sensory integration framework it enhances the emergence of:
Attention & focus
Self-regulation
Postural Control
Praxis (motor planning), balance & coordination
Fine motor skills
“Evenness” or more regulated emotional & behavioural responses
Oral motor control and improved eating habits
Communication, articulation and social skills
Increased engagement and interaction, development of play skills
Visual motor integration
Improved sleep patterns
Toilet training
Beyond Music, The Science Behind The Listening Program

People often ask, “What makes The Listening Program so effective, and how is it different from regular music or other programs?” In this article, we make it easy for you to describe the unique psychoacoustic modifications of TLP in simple and applicable ways to your clients. One modification to call attention to is Spatial Surround™, which simulates the natural environment by allowing the listener to experience the movement of the music in all directions, stimulating and integrating both sides of the brain, and maximizing the benefits in each session.
The Listening Program® is a neuroscience-based music listening therapy for achieving optimum brain health and functioning and all you have to do is put the headset on your children and let them listen to the healing sounds of nature and neuro-engineered music selections from Advanced Brain Technology. They are currently offering a 7 day free trial.
The Listening Program® is not like any music you’ve heard before. It’s more than music. It’s music that works—to improve your mental, physical, and emotional health.
All TLP music has been painstakingly recorded and engineered and features performances by world-class musicians including the award-winning Arcangelos Chamber Ensemble (under the musical direction of Richard Lawrence) and composer and master ethno-percussionist Nacho Arimany, among others.
Using the highest audio quality recording technology (high-definition sound) and advanced neuro-acoustic techniques, TLP music has been acoustically modified to train your brain. It strengthens neurological pathways so you can improve your ability to learn, communicate, and process information.
TLP can benefit most anyone, and applications are wide ranging, from rehabilitation to wellness and peak performance. TLP can be used in schools, hospitals, therapy clinics, assisted living facilities, companies, athletic and music programs, in homes, and on military bases—and more.
To view or purchase a poster on the benifits of TLP with accumlative stress
CLICK HERE
CLICK HERE
For more programs for nuero-divergant individuals from Advanced Brain Technology, click on the links below.
For more on Sensory Processing please refer to the following great posts:
What is SPD? by Lemon and Lime Adventures
Ideas for how to cope with SPD by Golden Reflections Blog
Identifying SPD signs by Kim’s Counseling Corner
Myths about SPD by The Inspired Treehouse
Sensory Interventions at Home
As a very observant parent, you will notice or observe and then make notes in a journal of any sensory irregularity and anomalies that are unique to your child or different than the norm. Most children develop their own bio-rhythm and you can notice and record difficulties controlling energy levels or ability to play cooperatively or focus, as well.
If meltdowns are occurring after your child experiences certain feelings or triggers, then note the perceived cause, the behavior, responses or sensory interventions that did or did not calm them. You should see a pattern developing and then you can teach your child better responses.
It is very important to closely observe your child and take note of the following to help design a “diet” that is right for your child:
Times of day that are especially challenging
Response to transitions between settings and tasks
Activities and routines that your child over-reacts to or avoids
Activities that your child engages in for extended periods
Preferred activities
Challenging behaviors during meals or daily hygiene
How your child reacts to clothing (fabric, sleeve length, etc.)
How he/she reacts to food texture, tastes, smells, temperature, etc.
Relationships with peers and adults
Times when your child is especially active or inactive
What is a Daily Rhythm Chart?
What is a daily rhythm and what makes it different from a schedule? Schedules are often rigid, encompass each moment of the day and follow a clock. A daily rhythm on the other hand is fluid and leaves time for spontaneity, while still providing a general pattern to our days.
A daily rhthm is much more flexible. Though the exact time at which things happen might change day to day, the general flow of events is quite similar, even season to season. For example, in summer, bedtime might be a bit later, but the events leading up to it remain the same. In the summer more free play will be spent outside, and walks might be quite a bit longer than in winter.
In a world so big, young children are often overwhelmed, but having a daily rhythm allows them a sense of control over knowing what comes next. This is empowering and comforting to them, and often for us as adults too!
A daily rhythm also allows us to move at a slower pace. Rather than pack in a bunch of events (even fun ones!) into a day, we can make sure there is plenty of time for free play. This allows children time to become engrossed in whatever they are drawn towards and to recognise and expect their bio-rythms to be adjusted by sensory interventions if they need it.
In our house, Hope needed some theraputic music when she woke up and most of the morning. She hated to put on or wear clothes. She cried like they caused her excrutiating pain. So it was her gentle time if the day. We created sensory or process art or swang or played outside. Mornings were all about things she loved to do plus organizing and focusing sensory strategies. We spent some time outside in freeplay or a walk. Then lunch and a nap with theraputic music.
Afternoons were about learning or experiencing something new together, boppy and floortime and visiting friends or running errands. She was cheerful and focused so it was a social time of the day. I usually planned some sort of workout or heavy sensory intervention to wear her out just before I had to get dinner ready.
When Daddy got home she loved to show him her art and what she learned. I studied and Russ and Hope played and played rambunciously until she needed to calm down with a sensory intervention,TV or a movie, Then storytime, sensory pats on her back while theraputic drifted her off to sleep.
View full-size
View full-size
View full-size
Following a daily rhythm allows for more flexibility than a strict schedule. No day is exactly the same, nor should it be. We travel and go on day trips and adventures. We have playdates and soccer class. Some events happen 1x a week and some 1x a month. Some are planned and some are spontaneous. A daily rhythm allows for this flexibility while still meeting everyone’s needs for routine. It also can allow for some sensory play to even up their energy levels.
How can you create a daily rhythm?
What works for one family doesn’t necessarily work for another. Your daily rhythm will look different than mine. If you are interested in creating one but don’t know where to start, first begin with the fixed aspects of your day (such as mealtimes, naps, or school) and then plan a rhythm around that. It also helps to jot down things you want to happen every day (e.g. periods for uninterrupted play, walks, reading) and add those in. There may be other things (e.g. art projects, baking together, library outings) that you make a specific day for each week, or just choose to do spontaneously. When creating your daily rhythm, try to avoid adding the times, at least at first. Focus more on the pattern of events, to reduce pressure and let the day happen organically.
I have included a template you can print to create a daily rhythm yourself! Click the image below to download.
Your child's sensory needs will change as their body grows and CNS develops and in response to the use of the sensory diet activities, accommodations, and strategies.
Sensory Seeker Checklist Free PDF Download
When Should You Start Sensory Play?
Sensory Overload in Children
Sensory Overload as a Mom
19 Common Sensory Triggers
26 Signs & Symptoms of Sensory Issues
What is the difference between sensory seeking and sensory sensitive?
Sensory Rhythms or "Diets"
In the end, the best way to identify your child’s needs in order to create their sensory plan or diet is to observe them. See what types of activities or experiences seem to help them stay focused and regulated.
An occupational therapist, Patricia Wilbarger, proposed the concept of sensory diets in 1995. It is my advice to talk to the child’s occupational therapist or other healthcare professional for guidance on creating a sensory diet that is tailored to the child’s individual needs.
This sensory diet template below will help you get started. If you’re not sure where to begin when creating a sensory diet for your child, we’ve got you covered!
I’ve been there. It can be an overwhelming task to try and figure out what activities to include in a sensory diet or when to include them in your daily schedule. I hope that this process can be a little bit easier for you with my help.
Free Sensory Diet Template
In this download, you will receive a one-page PDF with the template seen above. If you need assistance in filling out the document, see our post on how to make a sensory diet.
Simply print it out and fill in the specific events where you think the child can benefit from a sensory activity/tool. Make an inventory of the activities you believe to be beneficial for the child.
Then, put together a schedule of when each activity will be done throughout the day. And that’s it! You’re on your way to creating a sensory diet that will help the child feel more regulated and better able to cope with the demands of daily life.
Here’s my best advice when creating a sensory diet:
1. Start slow and gradually add in new activities as the child becomes more comfortable with the concept
2. Be creative and have fun with it! There are no hard and fast rules when it comes to a sensory diet, so feel free to get creative and tailor the activities to the child’s individual needs and interests
3. Involve the whole family! A sensory diet can be a great way to bond with the child and help everyone in the family learn more about how to support the child’s needs
4. Make sure to involve an occupational therapist or another licensed professional in the creation of the child’s sensory diet to ensure that it is safe and appropriate for their individual needs
Individual Sensory Diet or Plan Template